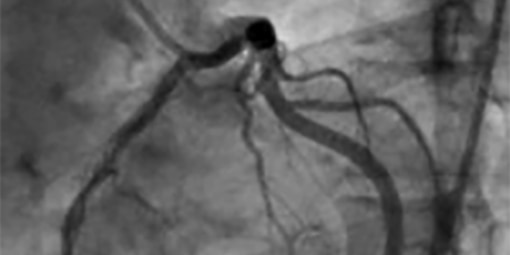
Coronary Angiogram / Angioplasty
Coronary angiography is an important test, usually used when your doctor suspects, knows, or definitively needs to rule out that you have coronary artery disease. Coronary angiography is when special types of real-time X-rays of your coronary arteries are taken. It shows your cardiologist if these arteries are narrowed or blocked.
Why do people need coronary angiography?
Your cardiologist may recommend that you undergo a coronary angiogram:
- if you have chest pain that your doctor suspects is caused by narrowed coronary arteries
- if your cardiologist wants to assess the degree of narrowing in your coronary arteries to see if you could benefit from angioplasty or bypass surgery, to relieve your symptoms and reduce your risk of further heart problems
- if you have had a documented heart attack – or you have continuing chest pain, or the results of an exercise test indicate the need for further investigation, your doctor will need detailed information about your heart and arteries
- as part of an overall work-up for a heart operation which may or may not involve concomitant by-pass surgery if your arteries are co-incidentally found to be narrowed (ie for heart valve surgery, it is always important to do an angiogram first)
Before your coronary angiogram, your cardiologist will discuss all the potential risks weighed up against the possible benefits. He or she will answer any questions that you or your family may have.
If you agree to have the procedure after discussing this with your cardiologist, you will be required to sign a consent form, which will be done either in the consulting rooms or in the recovery room just prior to your procedure.
WHAT HAPPENS DURING THE PROCEDURE?
During coronary angiography, you are given a local anaesthetic under the skin, and then a catheter (a long thin tube) is fed into an artery in your groin or your wrist. The catheter is moved up the inside of your artery until it reaches your heart. You will not feel any discomfort as these tubes move within the arterial system in your body. A special dye is then injected via the catheter into your coronary arteries and real-time X-rays are then taken. The X-ray image (‘coronary angiogram’) shows detailed information about your coronary arteries. It lets your doctor see if these arteries are narrowed, and if so, the degree of narrowing.
WHY DO PEOPLE NEED CORONARY ANGIOPLASTY AND STENTS?
- to improve blood flow to your heart if one or more of your arteries are too narrow because of significant plaque build-up
- if you have angina, because it can improve the flow of blood to your heart muscle by opening narrowed arteries
- if you have a heart attack, because it can help to quickly restore the flow of blood and minimise damage to your heart by opening narrowed arteries.
Other treatments for coronary heart disease include:
- medicine, which:
- can make your blood less likely to clot
- slow your heart rate
- make your blood vessels wider
- lower your blood pressure
- reduce your risk of having a heart attack and stroke
- bypass surgery, which:
- involves grafting a blood vessel from your chest, leg or forearm to your coronary artery to redirect blood flow around the most narrowed part of this artery
- lets your blood ‘detour’ past the narrowing to reach your heart muscle.
Your cardiologist will look at your symptoms and the results of your angiography test to help them to decide if angioplasty is suitable for you.
TYPES OF STENTS
Currently, there are 2 main types of stents.
Bare-metal stents (BMS) were once the commonest and only type of stent available. With the advent of the newer drug-coated stents, their use has reduced to patients who are at the lowest risk of restenosis occurring.
Drug-eluting stents (DES) are coated with a special medicine that is slowly released into your artery wall. This medicine stops tissue growing too much around the stent within your coronary artery. If the tissue grows too much it can make your artery narrow again (restenosis). Drug-eluting stents are therefore used to minimise the chance of restenosis in patients that are considered to be at higher risk for this. Hence, DES are used in smaller width arteries, bifurcating arteries, long narrowings, in diabetic patients, and to actually treat restenosis.
WILL ANGIOPLASTY CURE MY ANGINA?
Angioplasty is a very localised treatment, not a cure, for coronary arterial narrowings. It is not uncommon for such narrowings to grow immediately next to regions of the artery that have already been treated with angioplasty and stents.
For this reason, the best way to reduce your risk of more heart problems is to take your medicines as prescribed by your doctor and reduce or remove your ‘risk factors’ (things that increase your chance of developing coronary heart disease).
Other than taking your medicines as prescribed, the most important things that you can do are:
- refrain from smoking
- enjoy healthy eating
- be physically active
- control your blood pressure, and lower your cholesterol
- achieve and maintain a healthy body weight
- maintain your psychological and social health.
People with diabetes should aim to maintain their blood glucose levels within the normal non-diabetic range.
WHAT IS CORONARY ANGIOPLASTY AND STENTING?
This is a procedure that is usually undertaken with an almost identical preparation and sometimes immediately following a diagnostic coronary angiogram. It involves the cardiologist attempting to open up a significantly narrowed section of a coronary artery(s). Using similar tubes/catheters to a coronary angiogram, the cardiologist is able to manoeuvre a small balloon into the narrowing, inflating it to crush open the narrowing, and then removing the balloon and positioning a metal stent (hollow tube with side holes and struts) at the previous site of narrowing. Sometimes more than one stent is required to treat a particular area of the artery(s). Stents are used to prevent the elastic recoil of the artery at the site of ballooning, as well as to prevent re-narrowing at that site (termed ‘restenosis’).
Over time, the inside lining of your artery grows over the stent, so that the metallic support becomes part of the artery wall. If restenosis occurs, you may start to develop a recurrence of your initial symptoms (ie angina, shortness of breath). Restenosis of a stented area within your coronary arteries can be simply treated again with repeat stenting to that same area, or if there are other areas of narrowings, by-pass surgery may be required. Sometimes angioplasty and stenting is used in an emergency setting to treat a sudden heart attack, or myocardial infarction.
Moving catheters through your arteries won’t hurt you. However, you might feel transient chest discomfort when the balloon is inflated. This is because it temporarily blocks the flow of blood through your coronary artery.
